In May of 2019, immediately after receiving Federal Drug Administration approval for use, Novartis announced the price for their new one-time-use treatment for spinal muscular atrophy. The drug’s name was Zolgensma and the cost $2.1 m, making it the most expensive single dose drug in the world. Why is this?
Spinal muscular atrophy (SMA) is neuro-degenerative disease that affects 1 in 10,000 people. The main symptoms are muscle degradation and muscle weakness eventually developing into the inability to control voluntary movements including breathing and swallowing.
The cause is an alteration in the region of the DNA that contains the gene SMN1. SMN1 is responsible for producing the survival motor neuron protein that assists in the maintenance of motor neurons, that exist throughout the body connecting skeletal muscles, such as those found in the arms or legs, to the spinal cord. As the name suggests, the survival motor neuron protein is essential for the survival of motor neurons and the lack of or incorrect production of it results in neuronal death.
There are 5 sub-types of SMA resulting from SMN1 mutation. These differ in the types of symptoms that develop and the age at which they first occur. These range from type 4, charicterised by mild symptoms after the age of 30, to type 0 which occurs before birth and is fatal within the first year of life. The majority of SMA have parents which both carry a defective version of the SMN1 gene.
Historically, treatment has been focused on managing the symptoms of SMA, e.g. muscle relaxants and physical therapy to ease muscle tension. This improved the suffer’s quality of life but did little to tackle the underlying causes of the disease.
In December of 2016, a gene therapy called nusinersen, sold as Spinraza, was approved in the US and EU for treating SMA. It acts by targeting another gene, SMN2, that also contains information for producing SMN protein at much lower levels. This occurs because the intermediary messenger, the mRNA, contains a sequence that causes splicing factors, a group of regulatory proteins, to bind to it and stop it being correctly processed.
Spinraza binds to this mRNA sequence and stops the splicing factors binding. This allows the mRNA to be correctly processed and leads to the increased production of the SMN protein at levels which compensate for the reduced production by SMN1.
Spinraza is administered by an injection directly into the patient’s spinal cord so it can immediately be in contact with the motor neurons. Biogen, the manufacturers of Spinraza, recommend 3 initial injections, administered every 14 days, followed by another 5 weeks later. Maintenance treatment is also required in the form of a further injection every 4 months afterwards for the rest of the individual’s life.
The requirement for the maintenance treatment stems from the nature of the therapy. Both the SMN protein and the mRNA that encodes for it naturally degrade so are both in constant need of replenishment. Since Spinraza doesn’t alter the DNA and only in the mRNA that is produced from it there is a constant need for the drug to be present to bind and ensure the correct mRNA processing.
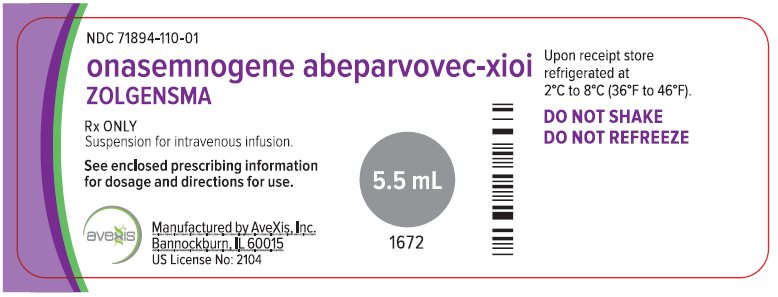
Zolgensma, developed by AveXis and sold by Novartis, is different in this regard as it directly acts upon the DNA and makes changes to the SMN1 gene and correcting it to the correct form. It thus eliminates the need for maintenance doses as any mRNA produced will be functional and lead to the production of the active SMN protein.
Gene delivery is achieved using a modified virus called AAV9, a which is known to not be pathogenic when used in humans and have a low immune response . The virus has part of it’s DNA replaced with the gene to be inserted and does so without inserting any viral or otherwise unwanted DNA.
In an early clinical trial, 15 children aged 6 months or younger with diagnosed type 1 SMA were treated with a single injection of Zolgensma. All were still alive at 20 months old and able to breathe without permanent mechanical assistance, compared to a 8% survival rate in historical cases.
There are issues with Zolgensma therapy. In the initial trial 1 of the initial 16 patients was removed from the trial because immune response related issues. In the remaining 15 patients 4 suffered severe side effects associated with the therapy.
There has also been some controversy surrounding the Zolgensma’s road to FDA approval. In August of 2019 it was reported that AveXis had submitted manipulated data to the FDA prior to receiving approval for use. Whilst the FDA didn’t have any concerns reagrding the safety of Zolgensma and stated that it should remain on the market it indicated that had it been informed earlier it would have delayed it’s approval decision to fully investigate.
This was followed up in October of 2019 by the halting of a clinical trial on the use of Zolgensma in older children due to concerning data from animal trials. As of writing the so called “STRONG” trial is still on hold despite 32 patients already receiving doses.
Despite the safety concerns and controversy, the day after the halting of the clinical trial Novartis announced that Zolgensma had $160 million worth of sales in it’s first quarter on the market. Biogen’s Spinraza meanwhile had $488 million in sales the same quarter.
The price for Spinraza is $125,000 per injection or $750,00 in the first year, and $375,000 every following year. So after the 17th injection or 4th full year of therapy Zolgensma is more cost effective. That is without including the costs to the healthcare provider for administrating the maintenance doses.
Furthermore, it has to always be remembered that drug development is an incredibly expensive process and any patent protection for the active drug expires at most 25 years after filling. In the case of Zolgensma, much of the initial development was performed by AveXis who were eventually bought by Novartis for $8.7 billion in April of 2018. Whilst there may be other factors in the acquisition, a large part of the assigned value would have been the potential value of Zolgensma .
SMA is classified by both the FDA and the EU as an orphan disease, a condition so rare that it is unprofitable to develop drugs and therapies. As a result drug development only occurs with support and subsidies from government agencies. That support it is often expected to be continued once the drug is launched at which point it’s up to public health bodies to decide if it provides “value for the taxpayer and benefits for patients.”
A combination of the rarity of the disease along with the immense difficulties required to produce such therapies is what gives Zolgesma it’s eye-catching price tag. Despite this and given that both Zolgensma and Spinraza appear to offer an opportunity at life for suffers of a truly terrible disease, they must both be considered incredible breakthroughs and every effort should be made available for to all eligible individuals by any means possible.